Department of Surgical Gastroenterology
The Department of Surgical Gastroenterology provides comprehensive, evidence-based care for benign and malignant diseases of the esophagus, stomach, small and large intestine, liver, gallbladder and biliary tract, pancreas, spleen, and abdominal wall, integrating advanced minimally invasive surgery with multidisciplinary perioperative pathways for optimal outcomes. Services span elective and emergency GI surgery, with protocoldriven management for acute abdomen, gastrointestinal bleeding, obstructive jaundice, pancreatitis, colorectal disease, and hepatobiliary-pancreatic pathologies, supported by standardized preoperative workup and enhanced recovery practices.


Endoscopy services
A fully equipped endoscopy suite provides diagnostic and therapeutic upper GI endoscopy and colonoscopy, including variceal ligation, ulcer hemostasis, polypectomy, foreign body retrieval, and stenting where indicated, enabling rapid diagnosis and minimally invasive intervention for acute and chronic GI conditions. Endoscopy workflows are integrated with anesthesia, pathology, and radiology to ensure timely biopsy, staging, and treatment planning for GI malignancies and complex benign disease.
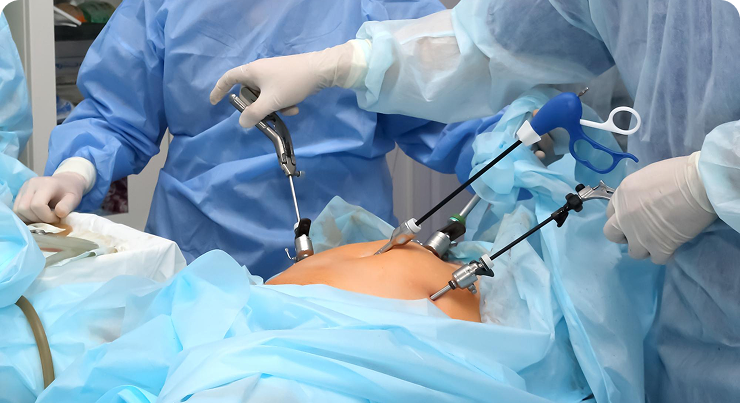
Laparoscopy and MIS
The department performs a wide spectrum of laparoscopic and minimal access surgeries with an emphasis on reduced pain, shorter stay, and early return to function, aligned with contemporary training and quality benchmarks in GI surgical practice. Advanced hernia services include laparoscopic TAPP, TEP/TEPP, and intraperitoneal onlay mesh (IPOM) repairs, alongside laparoscopy for cholecystectomy, appendectomy, adhesiolysis, colorectal resections, anti-reflux surgery, and select hepatopancreatobiliary procedures as per case selection.
Acute care and inpatient pathways
Emergency pathways support the management of perforation, obstruction, and GI hemorrhage with rapid resuscitation, targeted imaging, endoscopic hemostasis, and timely operative intervention when required, following national standard treatment guidelines. Inpatient care includes protocolized DVT prophylaxis, infection control, multimodal analgesia, early enteral nutrition, and discharge planning with clear follow-up and rehabilitation goals.
Education and quality
Structured academic activities include case conferences, journal clubs, morbidity and mortality reviews, and combined boards with medical gastroenterology and oncology, fostering competency in laparoscopic techniques, perioperative care, and GI oncology principles for trainees. Continuous audit and adherence to guideline-based care, coupled with community outreach and patient education, underpin the department’s commitment to safety, outcomes, and service to the region.
